Reproducing Innovation
This study provides an innovative underlying biomedical technology that has the potential to transform medical diagnostics through enabling repeated or even continuous measurement of biomolecules as individuals go about their normal day.
A key challenge for doctors treating hormone-related reproductive disorders is identifying the particular patients who could benefit from specific hormonal treatment. Now a combination of new robotics technology to measure hormone pulse patterns in the blood stream together with an innovative way of detecting hormones will improve diagnosis of reproductive disorders and lead to effective treatment for many patients.
Many common reproductive problems are hormone related. Altered pulse patterns of hormone secretion in the blood can lead to disorders such as polycystic ovary syndrome (PCOS), a condition that affects 5 to 7 percent of all women of reproductive age. Complications arising from PCOS and other hormone-related disorders can lead to infertility, metabolic syndrome and depression.
Accurately measuring these hormone changes to diagnose whether they are the cause of reproductive disorders has long been an elusive challenge for the medical profession. Hormone levels in the blood change constantly – even from hour to hour – which means relying on traditional blood tests is often insufficient for diagnosis.
A new joint collaborative study led by Dr Julian Tanner of the LKS Faculty of Medicine together with Professor Waljit Dhillo and Professor Tony Cass of Imperial College London has led to a new technology to meet this challenge. Dr Shaolin Liang was a joint PhD student between the laboratories at HKU and Imperial who developed this new approach during his PhD project to measure the pulse pattern of a key hormone called luteinising hormone.
“This study provides an innovative underlying biomedical technology that has the potential to transform medical diagnostics through enabling repeated or even continuous measurement of biomolecules as individuals go about their normal day,” Dr Tanner said.
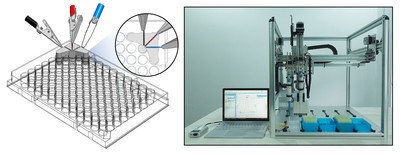
The team used a short piece of DNA called an aptamer which forms a particular shape when it specifically recognises the luteinising hormone. In the presence of the hormone, the aptamer changes shape. If the aptamer is on a conducting surface, one can measure the change in the electrical properties of the surface. In this way, the level of concentration of the hormone in a blood sample can be measured on a regular or ongoing basis. The electrochemical detector can also be connected to a robotic platform, allowing hundreds of blood samples to be measured at the same time and leading to reduced costs and increased efficiency.
The usual method of detecting the presence of a hormone is to use antibodies to search out a particular molecule, but this process causes irreversible changes to the molecule, cannot be digitised for analysis and can only be performed in central hospital laboratories. Using aptamers instead results in more repeatable, robust and less expensive detection. In the future, such a technology could underpin embedded sensors for real-time diagnostics to directly digitally monitor our health without the need to visit clinics.
This is one of the first times aptamers have been used in diagnostics, but it will not be the last. While the study only detects one molecule at a time, Dr Tanner expects future studies on diseases such as malaria to be able to detect multiple and possibly hundreds of molecules in one go, speeding up diagnosis and opening up many new potential improvements to monitor our health and wellbeing.